Unfortunately Tuesday was a rough day
Fortunately Wednesday was a brand new day.
On Wednesday I met with my Genetic Counselor Hallee. In any instance of Breast Cancer under the age of 45, you’re referred to a Genetic Counselor, and since my 23andMe results give a (very strong) indication that I will test positive for the BRCA1 mutation, they sped up my appointment to get me in ASAP.
Genetic Counseling is way more than just testing your blood and seeing what comes back. Halle started by taking a detailed family history, walking through my grandparents, parents, aunts & uncles, siblings and 1st cousins medical history (as it relates to cancer, which is mostly pretty boring). She even had a cool stencil to draw the tree out!
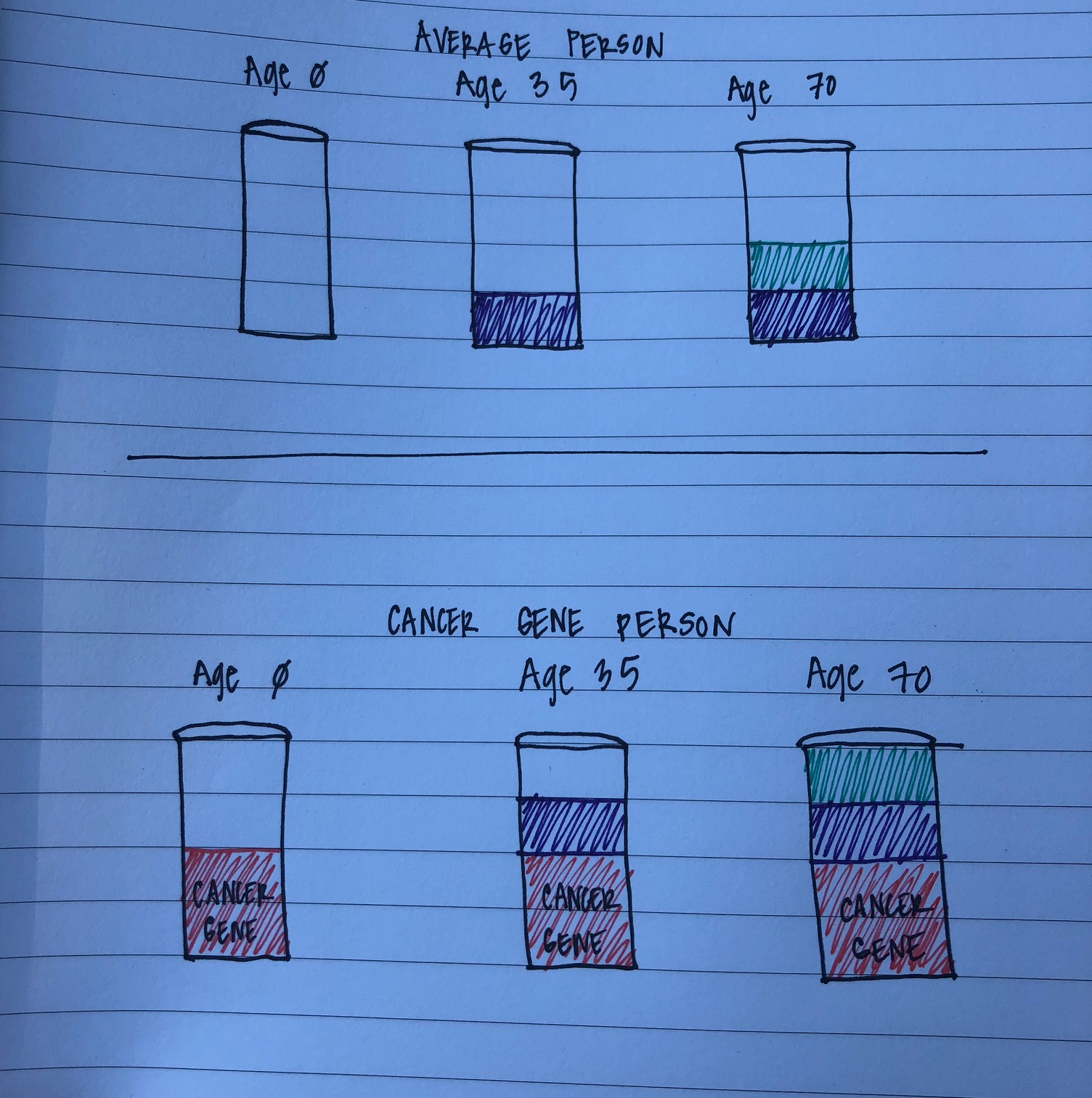
Before I get into the details of my specific genetic counseling, its worth a brief explanation of genetic mutations that predispose you to cancer (going forward referred to as a “cancer gene”), and the BRCA 1 mutation specifically. There are DOZENS of known genetic mutations that cause an individual to have a greater likelihood of developing certain cancers in their lifetime (and presumedly a whole bunch more that haven’t been “discovered” yet). Hallee explained how this works using a “cancer cup” analogy (picture below to help explain). An average person (one without a cancer gene) is born without any predisposition for developing cancer – their “cancer cup” is empty. Throughout their life, that person is exposed to a variety of factors that start to fill their cup up (flying on airplanes, smoking, sun exposure, etc. etc.) and the longer that person lives – and the more they choose certain behaviors – the more their cup fills up. In this analogy, when their cancer cup is “full” they have an incidence of cancer. An individual with a cancer gene is born with a cup that is already partially filled. The cup is not full ALL the way, meaning that they aren’t guaranteed to get cancer, but it takes less time to fill the cup up, and so this person is much more likely to get cancer in their lifetime, particularly at a younger than average age.
So, with this background on how cancer genes “work” – the specific cancer gene that i have is BRCA1 (BReast CAncer 1). This gene occurs in about 1 in 400 women in the average population, but among women of Ashkenazi Jewish decent, it occurs at a rate of 1 in 40. the BRCA1 gene can be inherited from either parent, and only one “copy” of the gene is needed for a child to inherit the gene. BRCA1 increases a woman’s likelihood of getting breast cancer in their lifetime by 60 percentage points (from 12% likely to 72% likely) and studies have shown BRCA1 also greatly increases a breast cancer survivor’s likelihood of getting breast cancer again (not a recurrence of the original cancer, but a brand NEW cancer). Additionally, BRCA1 increases the likelihood of getting ovarian cancer in one’s lifetime, from 1.3% to 44% (oof!). These statistics then factor in to treatment recommendations, not just to deal with the current cancer, but prevent future incidences of cancer going forward.
Its fairly rare for a BRCA 1 carrier to have no family history of breast, ovarian or prostate cancer, but after drawing out the family tree, Hallee could start to explain for why that rare occurrence was true in my case: I have a REALLY small family. My parents only have 3 siblings between the two of them, and I only have 4 first cousins across both sides of my family (while small, the Breier’s and Gavzy’s are both pretty mighty, so I’m happy with what I’ve got). Anyway, back to the genetics – in a small family with a genetic mutation that predisposes for cancer while each individual is more likely to develop certain cancers, with less total family members there is a lower likelihood that one of them will develop cancer. I’m not going to go into the further stats here because:
- Its boring
- I probably would mess it up
So my basic explanation will have to suffice. Even though 23andMe confirmed my BRCA1 status, Hallee wants to re-confirm in a medical environment – its less about not trusting the 23andMe results, and more having to do with getting the results to be part of my official medical file. Additionally, Hallee recommended that we do a full cancer-genetic screening panel – there are a number of other cancer genes, and if I happen to have more than just BRCA1, this would also impact long-term treatment recommendations.

So, I got my blood drawn – I have never been more appreciative of the Memorial Blood Center phlebotomists who never seem to have trouble finding a vein in my arm, which has unfortunately not been the case for the technicians drawing blood and inserting IVs over the last week. If you see me next week, check out my Wisconsin shaped bruise on my left arm – I’m hoping it fades by the start of football season so no one misinterprets my allegiances (GO BLUE!)
Side note – one of the ways you could indirectly “help” me is by donating blood, if that’s your jam (if not, I totally get it, there are other ways to help that don’t involve needles and bodily fluids). I’m not likely going to need blood, but my diagnosis and impending treatment means I won’t be able to donate blood every 8 weeks like I normally do, so if you wanted to be my blood donation “fill-in” that would be pretty cool (bonus points if you’re O+ like me!)
Anyway, my blood is off to the lab for genetic testing, with initial results in within the next week or two, and full results in by the end of the month. Some of you might be wondering “but what about your family? isn’t this genetic?” (these “some of you” I mention are probably said family). Hallee also discussed who in my family should get tested. Basically, because of the prevalence of BRCA1 in Ashkenazi Jews, its likely that my dad also has BRCA1 (along with its own set of cancer cup impacts). Related, this article from Haaretz, an Israeli news-media company, outlines some really interesting tidbits about Jewish genetics and why there is such a prevalence of certain genetic mutations in this population – don’t worry the article is in English! Anyway, men with BRCA1 are also at an increased risk of Breast Cancer (yup, dudes can get boob cancer!) but the rates of breast cancer in men are SO low, that an increased rate still means its fairly unlikely. Anyway, my dad will get tested, and if he’s the carrier, we’ll move to other members on his side of the family so that they can get tested as well – if they want. That will likely all happen throughout the fall.
So, you now know about what I know in terms of cancer genes. Hallee was helpful in providing the medical recommendations for a BRCA1 carrier that has breast cancer. Long story short, because of my genetic pre-disposition to breast and ovarian cancer, when I have my post-chemo surgery, I’ll have a prophylactic double mastectomy – where a non-cancer-gene patient in my shoes might be able to get by with just a lumpectomy. This will GREATLY reduce my chances of future breast cancer (although not entirely). We won’t get into the nitty-gritty on all that here until surgery is closer in the late-fall / winter time frame. Additionally, the medical recommendation is to have a prophylactic oophorectomy between the ages of 35-40 (preventative removal of the ovaries – also a hilarious sounding set of words – seriously, say it out loud, its like a party for your lips!). When surgery time gets closer, I’ll discuss with my surgeon whether it makes sense to do this in the same surgery as the mastectomy, or as a separate surgery later on (but sooner rather than later). Long story short – my genes lead us down a specific surgical path, but one that will follow chemo.
Unfortunately my genes are kind of jacked up.
Fortunately my jacked up genes have been studied a TON by medical professionals, so we know what to do about them!
As always, thanks for sharing Ari. Knowledge = POWER & Choices, so I am glad that you learned so much about next steps. Still, I can only imagine that hearing all of that left you with a very full brain and heart. Hugs, lady…we’re with you!!
LikeLike
I was diagnosed with Lynch Sydrome, specifically the MLH1 mutation, earlier this year. The amount of information is overwhelming! I had my hysterectomy in April and now need to get going with my own genetic counseling appointment, and also a colonoscopy at age 35. Can’t wait… Good luck ot you on your journey!
LikeLike